To Be Prepared (or Not to Be)
- Lorrie D. Divers, President, QRCP Solutions, Inc.
- Mar 9, 2018
- 3 min read
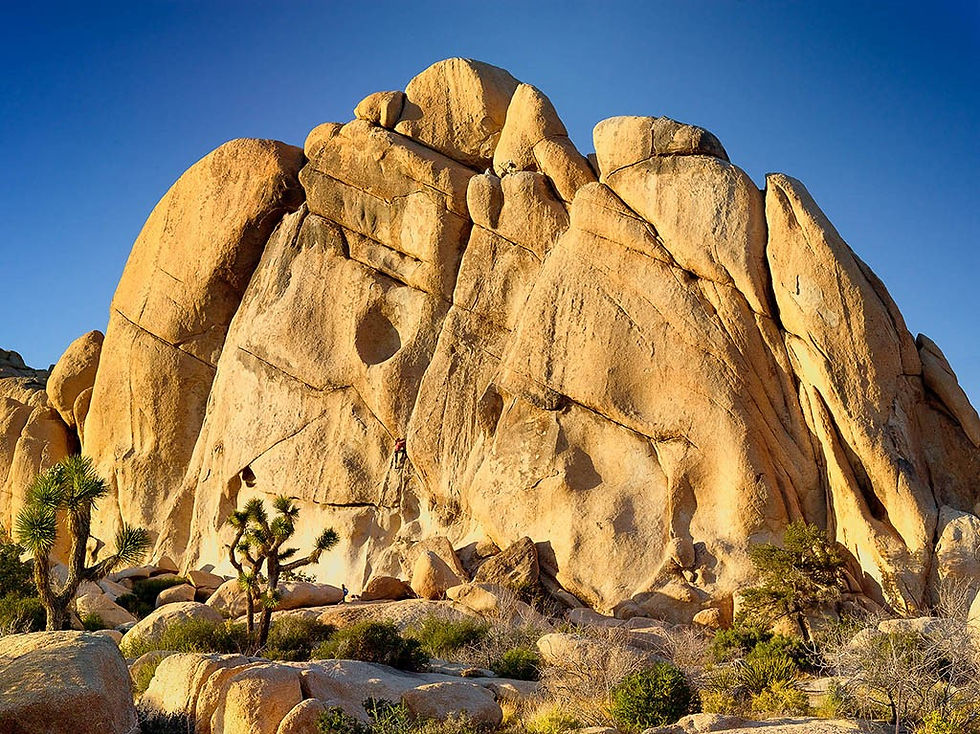
Earlier this week, I posted a quote about preparation and failure. While it might seem like a trite adage courtesy of Benjamin Franklin, I believe preparation is a good idea for everything from rock climbing to filing taxes. And of course, careful planning is critical to a successful clinical trial.
In two previous blogs [31-Jan-18, Risk Averse? and 8-Feb-2018, The Only Thing You Have to Fear Is…], I discussed risk assessment and risk management, including the concept of risk management plans. That latter term may be a bit misleading as it seems to imply a separate document specifically called a ‘risk management plan’ is required.
But to be truly effective, risk management must be organic throughout the clinical research and development process, including while planning and conducting clinical trials. Section 5.0 of the ICH E6(R2), recently published as a final guidance by the FDA, states, “The quality management system should use a risk-based approach as described below.” It goes on to highlight seven key components of this approach in Sections 5.0.1 through 5.0.7.
This key GCP guidance explains that Sponsors must plan (be prepared) to manage risk at both the system level and the clinical trial level, and the risks should be evaluated “against existing risk controls” for likelihood, detectability and impact. Control (management) of the risks should be, “proportionate to the significance of the risk.” But a separate thing called a ‘risk management plan’ is not expected for every individual risk in every clinical trial.
The guidance itself recognizes that many types of documents and activities provide information relevant to risk management. Section 5.0.4 clearly states, “Risk reduction activities may be incorporated in protocol design and implementation, monitoring plans, agreements between parties defining roles and responsibilities, systematic safeguards to ensure adherence to standard operating procedures, and training in processes and procedures.”
In short, what is necessary for each clinical trial is:
Understanding its unique risks
Whether or not the current controls (systems, procedures, training, personnel resources) are sufficient, or
If unique risks exist and require study specific controls
Documenting the assessment and decisions
Sponsors, CROs and other vendors, always have (or should always have….) at least one, and often several, operational documents that govern each clinical trial – an internal project plan, a specifications document, a detailed written quality and/or operational agreement, a specimen management plan – and this is where risk assessment and risk management could readily (and may already) be documented for each clinical trial.
For example:
Sections in existing operational plans or agreements that describe applicable SOPs, including any study specific procedures, study specific training requirements, quality metrics and their tolerance limits, communication and escalation trees can all serve to document risks and their prospective mitigation.
A monitoring plan, a data management plan, and a statistical analysis plan should also be prepared for each clinical trial and would logically include risk related information, including risk controls for these critical activities. If you are not familiar with these three key documents, regulatory and best practices guidance is available.
SOPs governing these types of standard plans and agreements should mention that as part of their preparation, trial specific risks are assessed and their unique controls will be described where necessary.
All clinical trials quality and operational procedures should provide clear details for managing common, known risks with standardized controls. For example, the specimen management procedure should adequately cover the risks of inadequate specimen identifiers and their management by describing the minimum required identifiers and the process to query inadequate information, as well as the disposition of any unidentifiable specimens.
You may not think that kind of information in an SOP is ‘risk assessment’ and ‘risk management,’ but in reality it is (or it should be….), just at a standardized, systematic level, which is necessary for critical and repetitive tasks. Indeed, that is one of the key purposes of a standard operating procedure.
Risk management ‘plans’ can take many forms, but no matter what form they take (an SOP, a plan, an agreement) the most important aspects are that they:
Be realistic
Incorporate standard policies, practices and procedures whenever possible
Identify and control for study specific elements and their risks
Be accessible to personnel and used operationally
Be assessed for effectiveness and updated as needed
Be focused on maximizing actions, behaviors, systems and records that ensure the protection of the study subjects rights, safety and welfare, and the data integrity of the trial.
That is being prepared for a clinical trial!
Let’s start a conversation! Follow QCRP Solutions, Inc. on LinkedIn for more quality assurance, regulatory compliance and process excellence topics. Contact me at ldivers@qrcpsolutions.com to learn more about our services.
Image: By Doug Dolde at English Wikipedia [Public domain], via Wikimedia Commons




Comments